African-Americans have a distinct perception of depression, and it doesn’t line up with the classic signs and symptoms promoted by the American Psychiatric Association, a new study suggests.
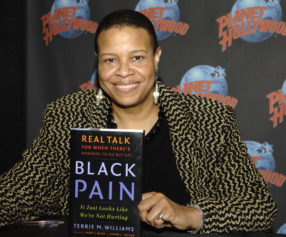
Sirry Alang, an assistant professor of sociology and anthropology at Lehigh University in Pennsylvania, spent an entire year in a predominately Black urban neighborhood in the Midwest to get a better understanding of the way African-Americans process the condition.
The researcher closely observed residents of the town, accompanying them to their homes, churches, community events and public streets, barber shops, hair salons and bus stops for informal interviews.
Her findings, published in the Social Science & Medicine journal, show that many do not view depression as a health condition at all. Alang found that Black Americans think of the disorder as a personal weakness that stands in opposition to the steadfast strength the community prides itself on.
The APA’s Diagnostic and Statistical Manual of Mental Disorders details standard criteria for the classification and diagnosis of mental health disorders, and it is the go-to source for physicians, researchers, psychiatric drug regulators, health insurance and pharmaceutical companies, the legal system and policy makers.
The manual outlines symptoms such as loss of interest in activities, insomnia or excessive sleeping, and inability to concentrate, but African-Americans in the study also experienced anger, agitation and the frantic need for human interaction.
“It is impossible to effectively diagnose and treat depression among African Americans if their perspectives about depression are not taken into account,” Alang noted in the media release.
She said that clinicians risk missing African-American’s unique symptoms by limiting diagnostic measures to those contained in the manual and recommended that practitioners educate themselves on assumptions about depression in the Black community so that they’ll be more likely to recognize markers.
On a positive note, Alang found that in the face of prevalent socioeconomic barriers, Black residents saw themselves as resilient.
Black Americans are 20 percent more likely to report serious psychological distress than the general population, and major depression is one of the most common illnesses, according to the U.S. Health and Human Services’ Office of Minority Health.
Experts have attributed the racial disparity to systemic disadvantages such as poverty, increased exposure to violence and homelessness, which Blacks encounter at disproportionate rates.
The OMH reports that Black adults living below the poverty line are two to three times more likely to experience severe mental health issues than those living above it, and Black adults are more likely to feel intensely sad, hopeless and worthless than white adults.
Other studies have shown that health care providers are part of the problem.
Princeton University doctoral candidate Heather Kugelmass found that psychotherapists regularly discriminate against prospective patients who are Black, regardless of socioeconomic standing. In the study, released earlier this month, voice actors posing as middle-class African-Americans with insurance were less likely to get a call back from therapists than whites with similar characteristics.
Georgia State University researchers found that psychiatrists were less likely to medicate Black patients with mental disorders, though they are almost twice as likely to be diagnosed with schizophrenia.