Black people are less likely than white people to receive CPR from a bystander after going into cardiac arrest at home or in a public place, a new report shows.
About 1,000 Americans’ hearts stop beating suddenly each day, according to American Heart Association. Research shows one out 10 people who experience cardiac arrest out of the hospital will likely survive. Black people have lower survival rates, however, compared to white people, research also shows. Bystander CPR could increase those chances of survival.

“When somebody goes down, one of the most important critical things you can do that can save lives is to start CPR,” Dr. Paul Chan, a professor of medicine at the University of Missouri and one of the authors of the study, said.
According to the study that was presented at the American College of Cardiology’s (ACC) 71st Annual Scientific Session, Blacks and Hispanics are 26 percent less likely to receive CPR from a bystander than whites when they go into cardiac arrest at home. The gap was even wider in public. The study shows Blacks and Hispanics had a 41 percent lower likelihood of receiving CPR from a bystander than their white counterparts.
Chan said disparities in treatment have been historically unaddressed. He attributes the gap in treatment to a lack of CPR training in Black communities. However, it does not explain why white people are also more likely to receive CPR than Blacks and Hispanics in their own neighborhoods.
“The elephant in the room is how much is race or racism playing a role in decisions about responding to somebody in trouble when it occurs in public,” Chan said.
Researchers examined more than 110,000 out-of-hospital cardiac arrests from 2013 to 2019 and compared them to bystander CPR rates. About 80 percent of the minority cohort were Black, Chan said.
The data from the Cardiac Arrest Registry to Enhance Survival shows a white person going into cardiac arrest in a neighborhood where the population is more than 50 percent Black and the Hispanic was still more likely to get bystander CPR than a Black or Hispanic person who lives in that neighborhood.
While the study did not examine why the racial difference is prevalent in both white and minority neighborhoods, Chan notes that implicit bias or explicit bias most likely plays a part.
“Maybe when a white person collapses in a Black or Hispanic community, there are fewer assumptions about why they collapsed and what they need,” said Chan, who dedicates part of his work to Black and minority communities.
The research doctor also noted he does not have enough information to draw a conclusion, and the questions raised by the study have often gone unanswered.
“It’s usually somebody you don’t know. It’s somebody you’re walking by and you see somebody collapse in the streets,” Chan said. “It turns out that there may be a component of implicit if not explicit bias, and that may not just be harbored by individuals in white communities. There are issues of public safety, and I think everybody has some biases about individuals in their own communities.”
Rates of CPR training are undoubtedly lower in Black neighborhoods. In 2013, Chan and his colleagues found the annual rate of CPR training was lower in the counties in the South, those with higher proportions of rural areas, and of Black and Hispanic residents.
Chan said CPR training would be more accessible if it was free, especially in poorer neighborhoods. However, free CPR classes would not make a difference until Black residents understand how critical the life-saving technique is. It first needs to be “normalized” in Black communities, he said. But despite the glaring disparity, the American Red Cross, the American Heart Association and other health care organizations do not market CPR training to Black or brown people.
“Most of the pictures depict white mannequins and white responders,” Chan said. “I think we need to start thinking and discussing more critically and creatively about making sure that we balance the playing field.”
One way to address the issue, Chan said, is to bring CPR to where people already gather in neighborhoods, such as churches or barbershops. The approach also needs to be widespread, he said.
“I think that it needs to be systematic effort and a coordinated effort to really make CPR training more accessible,” Chan said.
The health community has made similar strides in tackling health care disparities.
The American Heart Association has an initiative called the Hair, Heart & Health that trains barbers and hairstylists to screen their clients’ blood pressure and obesity levels in their shops to help detect those at risk for heart disease and stroke and other diseases.
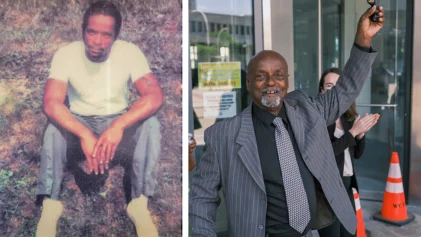
Anthony Pettiford, owner of United Barbershop in Greensboro, said the program created an opening to educate Black men about the importance of preventative care.
“Once you bring awareness, hopefully they pick up or may become concerned about their own personal health,” Pettiford said. “You try to put that on the floor to let them know the importance of health.”
Still, Chan pointed out that training can only cure the racial gap that may exist at home and not in public settings.
“We need to have a broader conversation about biases,” Chan said.